The Three Bodily Balance Systems: A Quick Overview
Updated: 12/28/24
Essential Points:
Balance relies on three main systems: Visual, somatosensory, and vestibular systems all contribute to maintaining our sense of balance, each processing different types of sensory information and sending signals to the brain for coordination and adjustment.
System failure can lead to instability: When one of these systems is impaired, the others compensate to maintain balance. However, if they cannot fully compensate, a person may experience unsteadiness and a higher risk of falls.
Balance rehabilitation focuses on system adaptation: Therapists can help individuals improve balance by adjusting the input of each system, either by challenging one system or enhancing the others, to support better coordination and stability.
In this article we will explore, in surface level detail, the three bodily balance systems. If you would like to learn more about each system scroll to the bottom of the sections for links to more robust and fleshed out articles on each system. Enjoy!
What Controls Our Balance?
When you think of balance, what comes to mind? Do you think of standing on one foot like the Karate Kid? Do you think of the famous French tight rope walker Philippe Petite? Maybe you experience an unnerving anxiety or a serene calmness? Whatever your first thought is, push it out of your brain, then ask yourself this question: What is balance?
For most, I would say that this is a simple question. We all on some level understand what a state of balance is. In a very unscientific answer one might say, “balance is the ability to not fall over”. A more studious answer may fall along the lines of, “balance is a bodily state of equilibrium and control”. At the heart of the matter both answers would be correct, but now pause for a minute and let us take it a step further. Ask yourself one more simple question: What controls our balance?
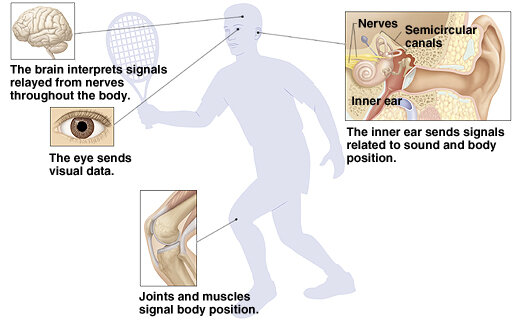
When it comes down to the brass tacks there are three major shot callers for balance. We will call these the three bodily balance systems: visual system, somatosensory (sensation) system, and vestibular (inner ear) system.
These three systems each individually take in a different type of stimulus from the outside world and send it to the brain for integration and processing. Once these sensations are integrated and understood by the brain, they are then sent through the nerves to the muscles for a proper response. If everything is in working order, our body is then able to make the appropriate adjustments based on the situation and maintain a sense of balance.
Of course, as you may already know, these systems can fail us. When one system fails the other two pick up the slack. If they are sufficient, our sense of balance is preserved. If they are not sufficient, we become unsteady and increase the of risk of falling.
For example, a 40-year-old healthy woman recently lost her eyesight due to an unfortunate accident. As a result, she no longer receives stimulus from her visual system. She now must rely solely on her somatosensory and vestibular systems to remain upright. At first, she will most likely feel very unsteady and unsafe because these two remaining systems were not prepared for this level of work. But, after a few weeks to months of forcibly training these systems to fire on all cylinders, the two systems learn to take up the slack and create a sense of balance in this woman.
So how do these systems work individually? Let us dive in.
The Visual System
The visual system, regarding balance, is the simplest system of the three bodily balance systems. It is purely made up of the eyeball and the optic nerve (CN II). This system works whether color blind or not, because it is all about depth perception and spatial awareness.
The visual system works by taking in light (sensory stimuli) through the pupil and transmitting this outward sensory stimuli from the retina, to the optic nerve, and finally to the brain. Once in the brain, this sensory information is evaluated and integrated to help maintain our balance.
Although not in the realm of a physical therapist, the visual system can often become impaired due to natural aging, accidental injury, and neurological disconnection. These impairments may manifest themselves as blindness, visual neglect, visual field cuts, and strange visual disturbances (floaters, mosaic like vision). We as therapists, or health professionals, must recognize these impairments and refer out to an appropriate professional to rectify the impairment as best possible. Unfortunately, sometimes a visual problem cannot be corrected easily. We may need to help guide the patient through an adaptation period as their other two systems learn to fill in the gaps.
Sometimes during a course of balance rehabilitation, we want to disrupt the visual system (even if naturally unimpaired) to heighten the training effect of the somatosensory or vestibular systems. To do this we simply manipulate the variables that allow normal stable eyesight. Such variables may include eyes opened/eyes closed, eye movement with head stabilization, simultaneous eye and head movement, calm visual environment/chaotic visual environment, and object tracking for just a few examples.
For a deep dive on the visual system check out this article here.
The Somatosensory (Sensation) System
The somatosensory system in its purest form simply allows us to feel the environment around us and know where our body and joints are in space via skin receptors and proprioceptors. This system practically encompasses the entire body. That is, wherever there is skin or a joint, this system is at work taking in information, relaying it to the brain, and allowing adjustments to be relayed to the muscles as needed.
For example, let us say you decide to go hike the White Mountains in New Hampshire. As you start to ascend, the path becomes severely rocky. Your ankles and feet start to contort around the various uneven surfaces. For safety, you have been looking down to the ground the entire hike. Then your friend urges you to look at the view while you walk. Suddenly, your visual system is occupied, and your somatosensory system kicks it up a gear. You start to feel your right ankle is slightly everted and dorsiflexed (proprioceptors at work) while planted on a rock. The sharp edges of the rock begin to dig into your shoe, and you feel a sense of friction and security (pressure/skin receptors at work). You then step with your left foot onto a mossy rock that is slick from the morning dew. Your sensory system sets off an alarm alerting you of the lack of friction allowing you to immediately course correct and plant your right foot down fast to a safe location to save you from slipping. You think nothing of it and continue enjoying the beautiful weather and view.
Imagine one simple change to the scenario, you have neuropathy in your feet leading to practically no sensation. Abruptly, your vision and somatosensory systems are offline in regard to the current task. The slick moss was never felt, and you slip. Lucky for you, you self-correct with a few arm and hip movements accessing the vast array of proprioceptors in your body to find a space of equilibrium. Of course, the vestibular system kicked in as well to add additional help. In the end you had a small scare, but the rest of the day is perfect.
Both scenarios took mere seconds, with millions of signals being transmitted between the body and brain like a sensory superhighway. Of course, as shown in the second example this system can also become flawed for various reasons including disease, scarring, previous injury, and neurological impairments to name a few. Again, we as therapists, will not be able to do much if the sensory system is impaired in terms of treating the impairment itself. What we can do though is recognize the impairments and refer out as appropriate all the while building up the other two balance systems.
Just like the visual system, sometimes we want to purposely impair the somatosensory system to train the remaining two balance systems. The main way of doing this is to change the surface a person is standing on to severely challenge this system and down regulate its effectiveness. Often therapy departments will use foam, air filled discs, and fancy balance toys to get the job done. Surfaces such as thick carpeting, grass, and sand work just as well too.
One last note, it almost sounds contradictory, but we also get to train the somatosensory system in these situations as well even though we temporarily down regulated the effectiveness of the system. Any new challenging surface contributes massive amounts of sensory information to the body essentially making the sensory receptors work overtime. Practice on these surfaces barefoot, and you basically just sent your nerves to sensory bootcamp as they must learn and adapt to the new signals coming in.
For a closer look at the somatosensory system check out this article here, or for a more intricate look at proprioception read this article here.
The Vestibular (inner ear) System
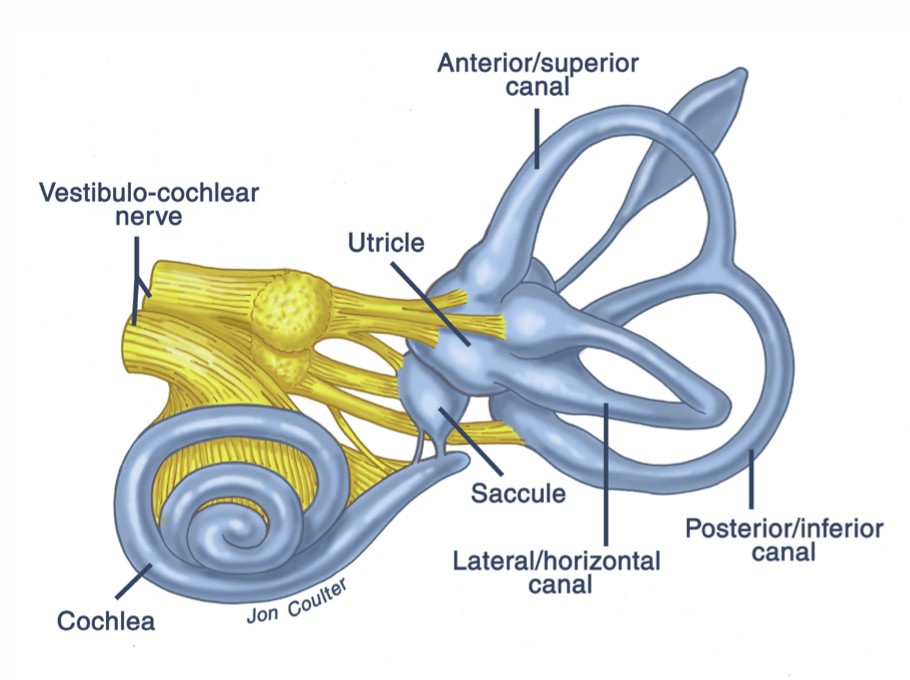
The vestibular system, in my humble opinion, is the most complicated of the three bodily balance systems. This system consists of sensors in the inner ear that are sensitive to motion and position of the head that then communicate with the vestibulocochlear nerve (CN VIII). In simple terms this system tells a person if their head is level and which direction they are moving. I will give a very brief overview of this system here, but I intend to write more in-depth articles in the future.
Rotational information occurs in structures called the semi-circular canals. There are three of these canals per ear named the superior, horizontal, and posterior canals. Each of these canals is filled with a fluid called endolymph which, when the head is rotated on its axis, moves, and shifts a structure called the ampullary cupula which in effect activates sensory receptors called hair cells. These hair cells then send a signal to the brain resulting in integrated rotational movement information. This sensory activation continues until rotational movement is halted bringing the system back into equilibrium.
Linear acceleration, as well as static head position awareness, arises from a structure called the vestibule, which is made up of the utricle and saccule. These structures work in a similar fashion to the semi-circular canals, but use weighted crystals called otoliths embedded into a gelatinous membrane. When linear motion occurs, these crystals shift the gelatinous membrane resulting in hair cells being stimulated. Static head position is also signaled similarly with the help of gravity pulling on the weighted crystals in various positions. Again, these hair cells send signals to the brain allowing linear motion and head position information to be integrated and understood.
When the vestibular system malfunctions pathology such as Ménière's disease or BPPV (benign paroxysmal positional vertigo) can occur. Consequently, a person may feel various symptoms including dizziness, nausea, hearing impairments, and vertigo. Depending on the root pathology, a physical therapist may be able to treat the pathology directly or may need to refer out to another specialty.
Just like the other two bodily balance systems, we as therapists often purposely impair this system to create an increased training effect on the visual and somatosensory systems. Doing this can be as simple as adding head turns into the balance task. For my lower level patients, I often find a position they are stable in and have them perform a series of head turns or have them draw large shapes with their nose in the air. By incorporating these head turns, the semi-circular canals and vestibule become overtaxed and cannot accurately supply orientational information to the brain and body.
As stated previously the vestibular system is highly complex. If you want to learn more about vestibular system anatomy read this article here, or if you want to dive deeper on how it functions on a physiological level read this article here.
Conclusion
There you have it, a quick introduction to the three key players in balance. The visual, somatosensory, and vestibular systems are the targets of therapeutic interventions for those with balance impairments. The true subtly in rehabbing these patients is understanding how to effectively turn the metaphorical dial on how much each system is working at any one time.
Think of it this way to simplify the idea in your brain. The balance equation must always equal 100%. In a healthy adult, each balance system contributes roughly 33% at any one time. If we as therapists can master the art of dialing down one system, while ramping up another, we can efficiently guide our patient on the journey of fixing, or compensating for, a balance impairment.
Thanks for reading today’s article! Did you know about the three bodily balance systems? What are your tricks or favorite go to exercises for a patient with balance impairments? Comment your thoughts below.
Happy falling!