How Preventing Falls Saves Lives and Billions: A Look at the Hidden Economics of Falling
Prefer to listen? Play the podcast version of this article below!
Essential Points:
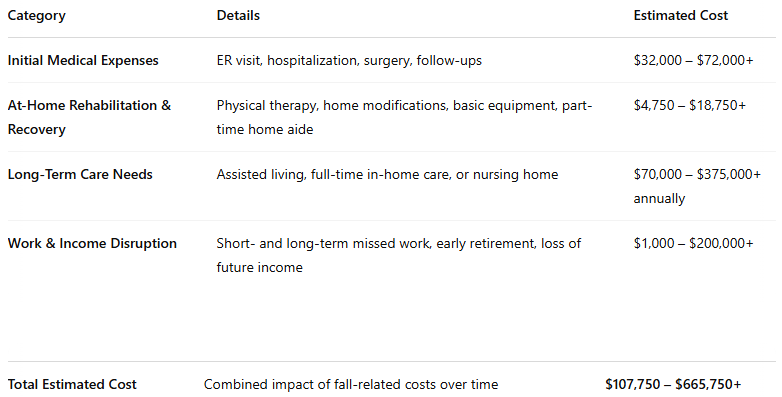
Falls aren’t just physical setbacks: They can trigger a financial disaster, with immediate medical costs ranging from $32,000 to $72,000+ in the first weeks alone.
Recovery often demands ongoing expenses: Physical therapy, home modifications, and caregiving support, can add another $4,750 to $18,750+ even after hospital discharge.
Serious falls can permanently alter your financial future: Early retirement, lost income, and potential long-term care costs can range from $70,000 to $375,000 per year.
Have you ever thought about what one slip, one misstep, or one moment of imbalance could actually cost you, not just in pain or recovery time, but in dollars and cents? It’s something most people don’t consider until it’s too late, or more bluntly, until their bank account is drained. But the truth is falling, especially as we age, can be financially devastating. Not just for you personally, but for the entire healthcare system we all rely on.
Whether it’s an emergency room visit, a hip replacement, or long-term care in a facility, the cost of falling adds up fast. And those costs don’t stop at medical bills. There’s lost independence, unpaid time off work (for you or a loved one who becomes your caregiver), home modifications, and the emotional toll of navigating a life changed overnight. It’s not an exaggeration to say that a single fall can set off a chain reaction, both physically and financially.
If we zoom out a bit, the picture gets even bigger. Each year, falls cost the U.S. healthcare system tens of billions of dollars. They are the leading cause of injury-related medical spending among older adults, and the numbers keep rising as our population ages. These aren’t just abstract stats, they represent real people, real families, and real financial strain on our economy.
But here’s the good news, most falls are preventable. And the financial burden associated with them? Also largely avoidable, with the right strategies, awareness, and action. That’s what this article is all about: taking a closer look at the economics of falling, both from your personal perspective and from a broader public health lens.
We’ll explore what a fall actually costs you out-of-pocket, how it impacts national healthcare spending, and why investing in prevention (whether it’s through exercise, education, or home safety) is one of the smartest financial decisions you can make as you age.
Welcome to the Economics of Falling 101, class is in session! Let’s break it all down.
The Personal Financial Cost of a Fall
Let’s start where it hits closest to home, your bank account.
When you picture the aftermath of a fall, you might imagine a bruise or maybe a cast, but behind those visible injuries is a financial ripple effect that can change your life overnight. A fall isn’t just a physical setback; it’s often the beginning of a cascade of unexpected expenses that can quickly drain your savings or sabotage your retirement plans. And unfortunately, these costs aren’t just hypothetical, they’re backed by the cold, hard math of healthcare billing that we all love so much.
Now, as a disclaimer, we all know that healthcare is one of the only industries that doesn’t give simple pricing for services until long after the service has been provided. Not only that, prices can fluctuate widely year to year depending on the healthcare company and the insurance you have. Throughout this article I will try and give a roughly accurate picture at the costs from a fall, but most numbers will be very rough averages, and those numbers can be drastically different based on your location and level of insurance. To create some semblance of uniformity, I’ll be using the high end of the US average costs I have found.
Out-of-Pocket Medical Costs Add Up Quickly
Even with good insurance, falling can still cost you thousands of dollars out of pocket. That’s because many plans include high deductibles, limited physical therapy sessions, or don’t cover home modifications and equipment that suddenly become essential after an injury. If you happen to be out-of-network with whoever is treating you, the cost can balloon out of control.
Here’s what the average cost breakdown might look like if you end up in the emergency room after a fall:
Emergency Room Visit: Between the facility fee and diagnostic tests like X-rays, CT scans, or MRIs, you’re often looking up to $4,000 just to get checked out. (1)
Hospitalization or In-Patient Stays: If the injury is serious, let’s say a broken hip or head trauma, admission to the hospital, or other in-patient facility, can be on average $18,000 or more. That’s potentially before any surgery or specialized treatment even begins. (2)
Surgical Procedures: A common fall-related surgery, like hip replacement, can cost anywhere from $10,000 to $50,000+, depending on where you live and what kind of coverage you have. (3)
Follow-up Appointments and Imaging: These appointments can vary significantly depending on your situation, but they may tack on another few hundred to thousands of dollars across multiple weeks or months as you heal and verify healing. Let’s assume an average basic visit with no imaging is roughly $140 and you need 3 follow-ups over a 6 month period. (4) That’s an additional $420.
Total Estimated Cost in the First Weeks After a Fall: $32,000–$72,000+
With that big of a bill, I hope you have good insurance! And that’s just the acute phase, the beginning of the story. Once you’re discharged from all in-patient related services, the costs don’t stop.
Rehabilitation and Recovery at Home: A Long, Expensive Road
After a fall, especially one that results in a fracture or head injury, recovery often becomes a full-time job. And unlike typical jobs, you’re paying to work. If you are lucky enough to head home after the hospital here is what you may be looking at:
Physical Therapy: Most people recovering from a fall or surgery will need multiple sessions per week for several weeks, or even months. At roughly $150 per session, that quickly adds up, especially if insurance only covers a limited number of visits per year. A typical hip replacement protocol requires PT for roughly 12 weeks with at least 2 sessions per week or more. (5, 6) If we do the math and assume a person just wants to function semi-normally and not get back to athletics that is $3,600 of PT.
Home Modifications: To make your environment safer post-fall, you might need to install grab bars in the bathroom, a ramp at the front door, or non-slip flooring. Depending on the scope of the work, you’re looking at a $1,000 to $10,000 minimum, with more extensive jobs drastically increasing the bill. (7, 8)
Medical Equipment: Even basic mobility aids like canes, walkers, or wheelchairs can set you back $50 to $500 or more, and you may need to rent or buy more than one piece of equipment during recovery. These costs can vary wildly, so lets assume a person needs a basic wheelchair and walker due to a moderate level injury. That would be roughly $100 for the wheelchair and $50 for the walker, totaling $150. (9, 10)
Home Health Aide: Depending on the injury and level of physical impairment, some people also require in-home health aides, which can cost $34 per hour and aren’t always covered by insurance. (11) A home health aide for 40 hours per week for just one month of their recovery would cost $5,000+. This would assume that the injured person is able to recover to a level of independence in one month which is often unlikely.
Total Estimated Cost for Home Recovery: $4,750 - $18,750+
These aren’t optional upgrades. They’re necessities if you want to avoid further injury and regain your independence at home. And for many people, they’re the first glimpse of how a fall can fundamentally shift the way they live (and spend).
Long-Term Care: When Independence Slips Away
Perhaps the most sobering financial consequence of falling is the risk of losing your independence. It’s a difficult subject we have to address, because for many older adults, a serious fall is the event that leads to a permanent move into assisted living or a skilled nursing facility. This is the world many of my own patients live in, and I see them deal with the financial fallouts every day.
Assisted Living or Nursing Home Costs: Monthly fees can range from roughly $6,000 to $31,000, depending on your location and the level of care required. Over a year, that’s $70,000 to $375,000, often out of pocket, especially if you don’t qualify for Medicaid or other price covering services. (12)
Home Care as an Alternative: Some people try to stay home with the help of caregivers, but round-the-clock care can cost just as much, if not more, than a facility. Home health aides make an average of $34 per hour, and a week contains 168 hours. (12) If a person needs 24/7 care that will be $22,848 per month, and $274,176 per year. If we assume a family member can support the person for at least 8 hours a day, that cost can come down to $15,232 per month, and $182,784 per year.
Total Estimated Cost if Independence Lost: $70,000 - $375,000
And even if you don’t require long-term care immediately, a fall often sparks a slow shift in your ability to stay fully independent. Driving may no longer be safe. Cooking becomes difficult. You might need help dressing or bathing. These changes mean new expenses, new dependencies, and sometimes, new living arrangements. The cost is nearly incalculable.
Loss of Income and Career Setbacks
Falls don’t only affect people over 65. If you’re in your 50s or early 60s and still working, the consequences of a fall can derail your career or delay your retirement plans.
Missed Work: A serious injury might take you out of work for weeks or even months. And if you're self-employed or don’t have paid leave, that’s not just time, that’s money you're not getting back.
Let’s put some numbers to it. The median household income in the U.S. is around $78,538. (13) Split between two adults, that’s roughly $39,000 per person per year. One month away from work? That’s a $3,272 hit to your income, not including medical bills, rehab costs, or out-of-pocket expenses like childcare or transportation to appointments.
Early Retirement: In more serious cases, a return to work might not be possible at all. That could mean tapping into your retirement funds earlier than planned, triggering penalties or diminishing the financial cushion you’ve worked so hard to build.
The average person age 65+ has around $600,000 in retirement savings. (14) Assuming no penalties, that gives you roughly $46,000 per year to live on over the average remaining lifespan of 13 years.(15)
Now, compare that to the average cost of a nursing home stay, over $70,000 per year. (12) Even if your fall pushes you into retirement at the usual age, that math already looks grim. But if you're forced to retire early, before you're financially ready, it gets even tougher.
Job Market Challenges: If you're lucky enough to recover from a serious injury, getting back into the workforce after a long layoff isn’t easy, especially if your job involves physical labor. Age discrimination is real. And the longer you're out, the harder it becomes to find work that matches your skills, needs, and physical limitations.
It’s tough to put this kind of financial loss into exact numbers, but let’s give it a try. The median U.S. household income is $78,538. (16) Assuming a two-adult household, that breaks down to about $39,000 per person per year.
Now imagine this scenario. You’re injured at 55, spend the next three years recovering, and don’t return to consistent employment until age 60. Over that five-year stretch, you could miss out on as much as $195,000 in lost income, and that’s before considering lost retirement contributions, raises, or compounding interest on investments.
Total Estimated Lost Income From a Serious Fall: $1000 - $200,000+
It’s a tough reality. One fall can rob you not only of your physical mobility but also your financial momentum.
The Hidden Cost: Burden on Family Caregivers
There’s also the often-overlooked economic impact on your family and loved ones. If you need help recovering, someone usually steps up, and that someone often sacrifices more than we realize.
Lost Work Hours: Family members who take time off to provide care may have to reduce their hours, use vacation or sick leave, or even quit their jobs.
Emotional and Physical Strain: Caregiving can be emotionally exhausting, especially when it’s sudden and long-term. This can lead to burnout, strained relationships, and even secondary health issues for the caregiver. (17) Many caregivers under high levels of stress actually have increased of mortality compared to non-caregiver counterparts. (18)
Out-of-Pocket Expenses: Many caregivers dip into their own funds to cover gas, flights, meals, medications, medical supplies, and living expenses that aren’t covered by insurance.
Total Estimated Cost to Family Caregivers After a Fall: Incalculable
It’s not just your own finances that are at risk, your fall can create ripple effects that touch everyone around you.
Final Total Estimated Cost From a Fall
When it comes down to it, there's no precise way to predict how much a fall will actually cost you or your family. The hard data is limited, and even when we do have numbers, the true financial toll depends on several key factors: your age, where you live, what kind of insurance you have, your support system, and the severity of the injury.
In many cases, trying to estimate the cost of a serious fall is like trying to guess the exact payout of a lottery ticket, only this time, you're not winning anything. You're trying to gauge how much you stand to lose. That said, we can still paint a picture based on the most likely scenarios. When you combine the immediate medical bills, rehabilitation, long-term care, and potential income loss, the range looks like this:
Total Estimated Cost After a Serious Fall: $107,750 - $665,750
As you can see, a single fall can wipe out decades of savings, derail your retirement plans, and put a financial strain not just on you, but on your loved ones as well. It’s not just a medical event, it’s a life-changing financial blow.
But remember, you're just one person. Thousands of people fall every single day. So what happens when we zoom out and look at the bigger picture? What kind of burden does this place on our healthcare system as a whole?
The Healthcare System’s Burden
If you’ve ever wondered why there’s so much concern about preventing falls in older adults, it’s not just about the personal impact, although that’s huge and of large concern. It’s also about the ripple effect that one fall can have on the entire healthcare system. Every time someone ends up in the ER with a broken hip or a head injury, the cost doesn’t just stop at the individual level. It echoes throughout hospitals, insurance companies, government programs like Medicare, and even the workforce. And when you multiply that by the millions of falls that happen each year, it’s easy to see how the economic burden of falls becomes an issue we all share, even if you’ve never fallen yourself.
Let’s break down just how deep this goes.
The Staggering National Impact of Falls
Let’s start with the numbers, because sometimes the cold, hard stats help us fully grasp the scale of a problem.
Over $50 billion dollars. That’s what Medicare and other healthcare programs spend every year treating non-fatal fall-related injuries in older adults. (19) Yes, billion with a “B.” To keep that in relative context, the US spends about $4.9 Trillion dollars per year on healthcare. (20) If you do the math, that means falls account for a little over 1% of yearly healthcare spend for direct costs alone.
More than 3 million emergency room visits happen annually because of falls in older people alone. (21, 22) That means that, every single day, thousands of people across the country are heading to the ER with injuries that are often preventable.
1 in 4 older adults fall each year, leading to both low level and high level injury. (23)
Hospital readmission rates are sky-high after fall-related injuries. (24, 25, 26) Once someone falls and ends up hospitalized, they’re statistically more likely to return to the hospital within weeks or months. That cycle not only drains the system financially, but it also slows recovery and reduces quality of life.
And it’s not just the U.S. that’s grappling with this. Globally, falls are one of the leading causes of injury and death in older adults. The World Health Organization reports that roughly 684,000 people die from falls every year worldwide. (27) It’s a massive, ongoing public health challenge, no matter where you live.
The Indirect Costs You Don’t See on a Bill
The direct costs like ambulance rides, hospital stays, surgeries, and rehabilitation, are just the beginning. The indirect costs of fall-related injuries are harder to quantify, but just as important, if not more.
Here’s what often happens behind the scenes:
Delayed discharges. Even when someone is ready to leave the hospital physically, they might not have a safe environment to return to. If the home isn’t equipped with grab bars, ramps, or other needed modifications, discharge gets delayed. That ties up beds for other patients and increases costs for the healthcare system as a whole leading to massive inefficiencies. (28)
Post-discharge services. Many older adults need ongoing help once they return home: physical therapy, visiting nurses, in-home aides, or meal services. While necessary, these services add to the long-term strain on both families and social service programs.
Strain on social services. Falls often push people into needing government aid they previously didn’t require, like Medicaid for long-term care or community resources for the disabled or elderly. While these systems were put in place for this exact purpose, they have become more strained in recent years for a multitude of reasons and now support 1 in 3 Americans. (29, 30) The long-term repercussions of this are yet to be seen.
These extended, complex care needs cause a cascading demand on healthcare resources, and those costs build up fast in incalculable ways.
Insurance and Policy Ripple Effects
You might think insurance would step-in and ease the burden, but I think over the last few decades many of us have seen what that reality actually looks like. While insurance can ease the burden of cost for some individuals, it doesn’t do so without longer term consequences.
When a fall leads to expensive treatments, surgeries, or rehab, that often translates into:
Increased insurance premiums across the board, not just for the person who fell, but for others in similar demographic pools due to the concept of risk-pooling. (31)
More claims for long-term disability. Serious fall-related injuries may leave someone unable to return to work, especially if they’re younger than retirement age. This creates potential strain on disability insurance programs and pushes people to access Medicaid earlier than expected.
Greater financial exposure for Medicare and Medicaid. As falls increase in frequency, especially with the aging Baby Boomer population, the pressure on these safety nets only grows. (32)
The bottom line is this: a single fall has financial consequences that extend far beyond the person who fell. And as our population ages, the cumulative effect could threaten the sustainability of healthcare systems if we don’t get proactive about prevention.
A Problem That’s Growing, Not Shrinking
Here’s what might surprise you most: the problem isn’t going away, it’s getting worse. The number of people aged 65 and older is projected to nearly double in the U.S. by 2060. (33) With age being a large risk factor for falls, we’re looking at a future with even more ER visits, surgeries, long-term care placements, and lost independence if we don’t act. (34)
And here’s where it gets personal: if you or someone you love is entering that high-risk age group, this isn't just a healthcare policy issue, it’s something that can hit close to home. Every fall that could have been prevented is not only a medical emergency but also a drain on your very own resources that could have been used elsewhere.
Whether you work in healthcare, policy, insurance, or are just planning for your own aging process, understanding the far-reaching impact of falls is key. It's not just about avoiding pain or hospital time, it's about protecting our collective future.
Falls Aren’t Inevitable & Prevention Saves Money
Here’s a truth that often gets overlooked: falls are not an unavoidable part of aging. They’re common, yes, but that doesn’t mean they’re inevitable. In fact, the vast majority of falls can be prevented with a bit of foresight, a few smart strategies, and often, a much smaller investment than the cost of treating an injury.
We’ve already looked at how expensive falls are for individuals, families, and the healthcare system. Now let’s flip the script and talk about something much more empowering, how prevention not only protects your health but saves serious money in the long run.
The Cost-Effectiveness of Fall Prevention
Preventing a fall is like plugging a leak before your whole kitchen floods. You spend a little time and money up front, a bit of hassle and spending of time, but you avoid the major financial and emotional damage that comes from ignoring the warning signs.
Here are just a few of the most effective, and affordable, fall prevention strategies:
Home safety assessments and modifications. Simple changes like installing grab bars, improving lighting, removing loose rugs, and adding railings can dramatically reduce fall risk. These upgrades typically cost between $1,000 - $10,000, depending on the size of your home and the level of work needed.
Balance and strength training programs. Programs like tai chi, balance-specific fitness classes, online balance programs, and physical therapy aren’t just for rehab, they’re proactive tools that retrain your body to stay upright. Many community centers offer classes for around $100–$200 for a series of sessions, online programs such as mine (check it out here) tend to run from $50-$100 total. Compare that to the cost of a hospital stay, and it’s a no-brainer.
Medication reviews. Certain prescriptions, especially sedatives, blood pressure meds, and antidepressants, can increase fall risk. These medications are often part of the BEERs Criteria. A pharmacist or physician can review your medications and help reduce dangerous combinations, a virtually free intervention with insurance that could save thousands of dollars over the long haul. (35)
Vision checks and proper footwear. Regular eye exams ($75-$200) and wearing proper shoes ($50-$100) may sound basic, but they’re foundational to balance. (36) Poor vision is a major contributor to falls, and proper shoes can prevent missteps and slips that lead to injury while enhancing your foot health and balance.
The key message? You don’t have to overhaul your entire life to reduce your fall risk. Small, intentional choices, especially when done consistently, can have a huge impact.
Prevention vs. Injury: A Cost Comparison
Let’s break it down even further. Here’s what a proactive approach looks like next to a reactive one:
Total Estimated Proactive Fall Prevention Costs: $1,175 - $10,600
Total Estimated Cost After a Serious Fall: $107,750 - $665,750+
Even on the conservative side, it’s easy to see how a few hundred dollars invested up front can prevent tens of thousands in medical bills, not to mention the emotional and physical toll of injury.
Prevention Isn’t Just Cost-Saving, It’s Evidence-Based
This isn’t just theory, it’s backed by science.
The CDC’s STEADI (Stopping Elderly Accidents, Deaths & Injuries) initiative provides clear guidelines and a toolkit for healthcare providers to screen, assess, and reduce fall risks in older adults. According to the CDC, implementing just a few of these measures can reduce fall rates by up to 24%, which adds up to billions of dollars saved annually in healthcare costs. (37) Another study published in the American Journal of Occupational Therapy showed that home modifications combined with physical activity programs significantly reduced falls and decline in physical function which would lead to fewer hospitalizations. (38)
And here’s something even more powerful: when fall prevention programs are embedded into regular health maintenance (like yearly physicals, Medicare wellness visits, or fitness coaching), older adults not only reduce their risk of falling but also improve overall wellbeing. (39, 40, 41, 42) That’s a ripple effect worth investing in.
Prevention Creates a Ripple of Independence
It’s not just about saving money, it’s about maintaining autonomy, freedom, and dignity for you and your loved ones.
When you fall, life gets smaller, much smaller. People become afraid to walk to the mailbox or take the stairs due to fear of falling again. Confidence in yourself shrinks, activity drops, and health declines. But when you build prevention into your daily life, through mindful movement, regular check-ups, and home adjustments, you send the opposite message to your body and brain: I’m still in control. I’m still capable. I’m still me.
And here’s the thing, fall prevention strategies are not just for “old” people. The best time to start is before you feel at risk. That’s when you’ll get the biggest benefit, and it’s why programs like my balance program are designed for people who want to age on their own terms, not just react to problems when they show up. Because YOU have all the power.
A Call to Action for Individuals and Policymakers
So far, we've covered the high stakes of falling later in life, the physical, emotional, and financial tolls, and we’ve made it clear that these aren’t just random accidents of aging. The good news is that there's a lot you can do, right now, to drastically reduce your personal risk or help someone you care about do the same. But meaningful, long-lasting change also needs to happen at a higher level, through the policies and programs that shape our healthcare and communities.
Let’s break down what that looks like on both a personal and societal level.
What You Can Do Right Now to Reduce Fall Risk
You don’t need to wait until something goes wrong to take action. In fact, the earlier you start thinking about fall prevention, the better your odds of aging with strength, confidence, and independence. Whether you’re in your 40s and planning ahead or already feeling unsteady on your feet, these strategies can make a real difference.
1. Get Proactive with Strength and Balance Training
One of the most powerful things you can do is start (or continue) a regular routine focused on balance, strength, and coordination. These aren’t just for athletes, they’re your body’s secret weapons against falling.
Strength training helps support joints and maintain bone density.
Check out my article on starting strength training here.
Balance training keeps your nervous system sharp and responsive.
Dive deeper into balance training with my articles on tandem balance and single leg balance to start your journey.
Coordination drills enhance reaction times, which are crucial during slips, trips, and stepping reactions.
The key is consistency, and the good news is, you don’t need a gym membership or expensive equipment to get started as much of this can be done from the comfort of your own home. Even 10–15 minutes a day, a few times a week, can dramatically change your long-term trajectory.
2. Check Your Home for Common Hazards
Most falls don’t happen out in the wild, they happen in familiar places like the bathroom, the kitchen, or even your bedroom. Fortunately, many of the biggest risks are easy to spot and inexpensive to fix.
Walk through your living space and look out for:
Loose throw rugs or cords in walking paths
Dim lighting, especially around stairs or doorways
Slippery surfaces in bathrooms or entryways
Lack of handrails or grab bars where needed
You can even bring in a professional for a home safety assessment, or use my starting guide on age proofing your home to assess your own needs right away.
3. Talk to Your Doctor About Fall Risk Factors
Falls are a medical issue, but many doctors don’t bring it up unless you do. So take the lead in your next checkup.
Ask about:
How your medications may affect balance, alertness, or blood pressure
When you last had a vision and hearing check
Whether physical therapy or balance assessments are recommended
If any underlying health conditions might increase your risk (like diabetes, arthritis, or neuropathy)
This isn’t about paranoia, it’s about building a smart, informed plan. Think of it like you would brushing your teeth to avoid cavities. Fall prevention is routine maintenance for your whole body.
What Society Needs to Step Up and Do
While personal action is critical, we also need systemic support. After all, not everyone has access to the same resources. A lot of people don’t even realize how close they are to being at risk until a fall changes everything.
This is where public health policy and community investment can make a major impact.
1. Fund and Expand Fall Prevention Programs
Many community centers, senior groups, and health organizations offer fall prevention classes, but often, they’re underfunded, under-promoted, or limited to certain age groups or income levels.
Government and nonprofit funding can change that.
Programs like:
Otago Exercise Program (an evidence-based routine for older adults)
Tai Chi for Arthritis and Fall Prevention
Matter of Balance workshops in community centers
…have been shown to significantly reduce fall risk. But they need support to scale up and reach the people who need them most.
2. Improve Access to Physical Therapy and Community Wellness
Physical therapy isn’t just for post-surgery rehab. It’s a essential tool for proactive care, especially when it comes to balance and gait training. Yet too many people miss out because of limited insurance coverage, location barriers, or simply not knowing it’s available.
Imagine a world where every primary care office had a referral pathway to a movement specialist, not just for athletes or injuries, but for aging well. We could prevent thousands of falls before they ever happen, and have a much more productive population.
Community wellness centers, walking groups, and accessible fitness spaces also make a huge difference. When people have places to move safely and joyfully, they’re more likely to stay active and mobile.
3. Include Fall Risk Education in Routine Primary Care
Right now, most adults don’t get screened for fall risk unless they’ve already fallen.
That needs to change.
Fall risk should be treated like blood pressure or cholesterol, something every adult gets checked regularly, especially after age 50. If a simple test or conversation could save someone from a hospital visit (or worse), why wouldn’t we make that standard?
Primary care providers should be trained and encouraged to:
Ask about previous falls or near-misses
Assess strength, gait, and reaction time
Educate patients about balance training and home safety
And importantly, these conversations need to happen without stigma. Falling isn’t a sign of weakness, it’s a signal that something in your system needs support. Catching it early is a sign of strength.
Final Thoughts: The True Cost of Falling
Falls are often brushed off as a normal part of aging, something to shrug off with a laugh and an ice pack if possible. But the truth is, the ripple effects of a single fall can be devastating, not just physically, but emotionally and financially. When someone you love falls, it can shift the course of their life. It can mean a fractured hip, a long hospital stay, the loss of independence, or the onset of fear that keeps them from enjoying the activities they once loved. It can mean depression, isolation, and a long, expensive road to recovery that doesn’t always end in a return to normal.
And this doesn’t just affect individuals and families, it affects all of us.
The financial cost of falls is staggering. According to the CDC, falls among older adults cost the U.S. healthcare system over $50 billion every year. That number is only projected to grow as our population ages. Much of this is paid by Medicare, Medicaid, and other public health resources, meaning taxpayers share the burden. Falls often lead to emergency room visits, surgeries, long-term rehabilitation, and in many cases, long-term care placement. This puts a strain on individuals, families, and an already overburdened healthcare system.
But here’s the part I can’t emphasize enough: most of these falls are preventable.
We have the knowledge. We have the tools. We just need the will to act, on both personal and societal levels.
So if you’re someone in your 40s, 50s, or early 60s reading this, the time to start thinking about fall prevention isn’t in your 70s. It’s now. If you’re a policymaker, healthcare provider, or someone who works with older adults, the time to invest in fall prevention programs isn’t when the problem is already urgent, it’s before it reaches that point.
As you walk away from this article, I hope you remember this one message:
A fall doesn’t just bruise your body, it can bruise your wallet too. But it doesn’t have to. Prevention is possible, and it starts with knowledge, movement, and smart choices.
References
Emergency department visits exceed affordability threshold for many consumers with private insurance - Peterson-KFF Health System Tracker. Peterson-KFF Health System Tracker. Published July 8, 2024. https://www.healthsystemtracker.org/brief/emergency-department-visits-exceed-affordability-thresholds-for-many-consumers-with-private-insurance/#Total%20and%20out-of-pocket%20costs%20by%20visit%20complexity%20code,%202019
Reider L, Falvey JR, Okoye SM, Wolff JL, Levy JF. Cost of U.S emergency department and inpatient visits for fall injuries in older adults. Injury. 2023;55(2):111199. doi:10.1016/j.injury.2023.111199
Procedure price lookup for outpatient services | Medicare.gov. https://www.medicare.gov/procedure-price-lookup/cost/27130%20,%20https://www.goodrx.com/health-topic/joints/how-much-does-a-hip-replacement-cost
Brooks A. Mira Health. Mira Health. Published February 25, 2025. https://www.talktomira.com/post/how-much-does-primary-care-cost-without-insurance
Ohio State Sports Medicine. TOTAL HIP REPLACEMENT POST-OP CLINICAL PRACTICE GUIDELINE. https://hrs.osu.edu/-/media/files/wexnermedical/patient-care/healthcare-services/sports-medicine/education/medical-professionals/hip/totalhipreplacement.pdf?la=en&hash=622323146BB495B688822D5126988FD59D669BA0
Department of Rehabilitation Services, The Brigham and Women’s Hospital, Inc., Department of Rehabilitation Services. Total Hip Arthroplasty/Hemiarthroplasty Protocol.; 2022. https://www.brighamandwomens.org/assets/BWH/patients-and-families/rehabilitation-services/pdfs/tha-protocol.pdf
Trout J. The Cost of Aging in Place Remodeling. Retirement Living. Published April 10, 2025. https://www.retirementliving.com/the-cost-of-aging-in-place-remodeling
Home Modifications: Use, Cost, and Interactions with Functioning Among Near-elderly and Older Adults. ASPE. Published October 9, 2008. https://aspe.hhs.gov/reports/home-modifications-use-cost-interactions-functioning-among-near-elderly-older-adults-1#result
Amazon.com : wheelchair. https://www.amazon.com/s?k=wheelchair&crid=183NAKIGM4O2C&sprefix=wheelchair%2Caps%2C164&ref=nb_sb_noss_1
Amazon.com : walker. https://www.amazon.com/s?k=walker&crid=7H1H9OJK0DFR&sprefix=walke%2Caps%2C172&ref=nb_sb_noss_2
Cost of long term care by state | Cost of care Report | Carescout. https://www.carescout.com/cost-of-care
Assisted Living Locators. Average cost of nursing home facilities | Assisted living locators. Assisted Living Locators. Published March 7, 2024. https://assistedlivinglocators.com/cost/average-cost-of-nursing-home-facilities#:~:text=How%20Much%20Do%20Nursing%20Home,nurse%20for%20in%2Dhome%20care.
United States Census Bureau QuickFacts. U.S. Census Bureau QuickFacts: United States. Census Bureau QuickFacts. https://www.census.gov/quickfacts/fact/table/US
Benson A, Sham J. What is the average retirement savings by age? NerdWallet. Published February 24, 2025. https://www.nerdwallet.com/article/investing/the-average-retirement-savings-by-age-and-why-you-need-more
Kochanek K, Murphy SL, Xu J, Arias E. Mortality in the United States, 2022.; 2023. doi:10.15620/cdc:135850
United States Census Bureau QuickFacts. U.S. Census Bureau QuickFacts: United States. Census Bureau QuickFacts. https://www.census.gov/quickfacts/fact/table/US
Kilmer G, Omura JD, Bouldin ED, et al. Changes in health indicators among caregivers — United States, 2015–2016 to 2021–2022. MMWR Morbidity and Mortality Weekly Report. 2024;73(34):740-746. doi:10.15585/mmwr.mm7334a2
Schulz R, Beach SR. Caregiving as a risk factor for mortality. JAMA. 1999;282(23):2215. doi:10.1001/jama.282.23.2215
Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical costs of fatal and nonfatal falls in older adults. Journal of the American Geriatrics Society. 2018;66(4):693-698. doi:10.1111/jgs.15304
Historical | CMS. https://www.cms.gov/data-research/statistics-trends-and-reports/national-health-expenditure-data/historical#:~:text=The%20data%20are%20presented%20by,For%20additional%20information%2C%20see%20below.
Facts about falls. Older Adult Fall Prevention. Published May 9, 2024. https://www.cdc.gov/falls/data-research/facts-stats/index.html
WISQARS Fatal and Nonfatal injury infographics. Centers for Disease Control and Prevention. https://wisqars.cdc.gov/infographics/
Older adult falls data. Older Adult Fall Prevention. Published October 28, 2024. https://www.cdc.gov/falls/data-research/index.html
Ayoung-Chee P, McIntyre L, Ebel BE, Mack CD, McCormick W, Maier RV. Long-term outcomes of ground-level falls in the elderly. Journal of Trauma and Acute Care Surgery. 2014;76(2):498-503. doi:10.1097/ta.0000000000000102
Fawcett VJ, Flynn-O’Brien KT, Shorter Z, et al. Risk factors for unplanned readmissions in older adult trauma patients in Washington State: A competing risk analysis. Journal of the American College of Surgeons. 2014;220(3):330-338. doi:10.1016/j.jamcollsurg.2014.11.012
Galet C, Zhou Y, Eyck PT, Romanowski KS. Fall injuries, associated deaths, and 30-day readmission for subsequent falls are increasing in the elderly US population: a query of the WHO mortality database and National Readmission Database from 2010 to 2014. Clinical Epidemiology. 2018;Volume 10:1627-1637. doi:10.2147/clep.s181138
World Health Organization: WHO. Injuries and violence. Published June 19, 2024. https://www.who.int/news-room/fact-sheets/detail/injuries-and-violence#:~:text=Falls%20account%20for%20over%20684%2C000,under%2Drecognized%20public%20health%20issue.
Rojas‐García A, Turner S, Pizzo E, Hudson E, Thomas J, Raine R. Impact and experiences of delayed discharge: A mixed‐studies systematic review. Health Expectations. 2017;21(1):41-56. doi:10.1111/hex.12619
USAFacts. How many people receive government assistance? USAFacts. https://usafacts.org/articles/how-many-people-receive-government-assistance/. Published September 24, 2024.
Rudowitz R, Burns A, Hinton E, Tolbert J. Medicaid: what to watch in 2025 | KFF. KFF. Published April 10, 2025. https://www.kff.org/medicaid/issue-brief/medicaid-what-to-watch-in-2025/#:~:text=State%20Budget%20Constraints%20and%20Priorities&text=Heading%20into%20FY%202025%2C%20revenue,and%20lead%20to%20program%20cuts.
Risk Pooling: How health insurance in the individual market works | American Academy of Actuaries. https://www.actuary.org/content/risk-pooling-how-health-insurance-individual-market-works-0#:~:text=What%20is%20risk%20pooling%3F&text=together%20allows%20the%20higher%20costs,stable%20the%20premiums%20can%20be.
Jones CH, Dolsten M. Healthcare on the brink: navigating the challenges of an aging society in the United States. Npj Aging. 2024;10(1). doi:10.1038/s41514-024-00148-2
Vespa J, Medina L, Armstrong DM. Demographic Turning Points for the United States: Population Projections for 2020 to 2060.; 2018. https://www.census.gov/content/dam/Census/library/publications/2020/demo/p25-1144.pdf
Appeadu MK, Bordoni B. Falls and fall prevention in older adults. StatPearls - NCBI Bookshelf. Published June 4, 2023. https://www.ncbi.nlm.nih.gov/books/NBK560761/
Robot or human? https://www.walmart.com/cp/medication-therapy-management/4851429
Plemons C. How much do eye exams cost? | eHealth. Published April 7, 2025. https://www.ehealthinsurance.com/resources/vision-insurance/eye-exams-importance-costs
Sarmiento K, Lee R. STEADI: CDC’s approach to make older adult fall prevention part of every primary care practice. Journal of Safety Research. 2017;63:105-109. doi:10.1016/j.jsr.2017.08.003
Chase CA, Mann K, Wasek S, Arbesman M. Systematic Review of the effect of home modification and fall Prevention Programs on falls and the Performance of Community-Dwelling Older Adults. American Journal of Occupational Therapy. 2012;66(3):284-291. doi:10.5014/ajot.2012.005017
Sherrington C, Fairhall N, Wallbank G, et al. Exercise for preventing falls in older people living in the community: an abridged Cochrane systematic review. British Journal of Sports Medicine. 2019;54(15):885-891. doi:10.1136/bjsports-2019-101512
Johnston YA, Bergen G, Bauer M, et al. Implementation of the Stopping Elderly Accidents, Deaths, and Injuries Initiative in Primary Care: An Outcome Evaluation. The Gerontologist. 2018;59(6):1182-1191. doi:10.1093/geront/gny101
Bs ALB, Becerra AZ PhD, Bs AM, et al. Medicare Annual Wellness Visit Association with Healthcare Quality and Costs. AJMC. https://www.ajmc.com/view/medicare-annual-wellness-visit-association-with-healthcare-quality-and-costs. Published August 6, 2020.
Ong MF, Soh KL, Saimon R, Wai MW, Mortell M, Soh KG. Fall prevention education to reduce fall risk among community‐dwelling older persons: A systematic review. Journal of Nursing Management. 2021;29(8):2674-2688. doi:10.1111/jonm.13434